Dear Dr. Zoomie – I’ve got a hot lab and I was told I need to develop a response plan in case someone gets skin contamination. I was thinking soap and water; is there anything else I should include?
Skin contamination doesn’t happen often but if you work with enough radioactivity – especially in liquid form (as in a hot lab) it’s going to happen from time to time. And it doesn’t mean that people are being careless and sloppy (well…sometimes it does, but not always); sometimes we just make mistakes. I’ve had skin contamination myself at least a couple dozen times – mostly just random splatters here and there – and every time it’s cleaned up fairly quickly with soap and water. But let’s back up a little bit and talk about what goes into dealing with skin contamination. Specifically, you need to have a procedure to follow, you need to know how to clean up the contamination (and how to know when you’re done cleaning up), and you have to know how to tell if any follow-up is required. Let’s take these one at a time.
Your skin contamination procedure doesn’t have to be very complicated; in fact, it only needs to have a couple of parts. It should:
- Define what’s meant by skin contamination. For example, you might define skin contamination as the presence of any contamination above background or you might decide that contamination levels have to exceed a certain limit (100 cpm above background, for example).
- Describe the steps to be taken when a person is contaminated. For example:
- Contact the Radiation Safety Officer at the earliest opportunity.
- Perform a count rate survey over the contaminated area and write down the number of CPM.
- Start to clean the contaminated skin in the nearest sink or at the nearest decontamination station.
- Discuss cleanup techniques (more on this in a moment).
- Determine when to call for outside assistance and/or follow-up (more on this later as well)
- Document what’shappened.
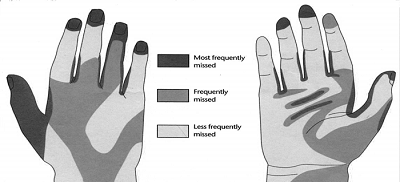
Cleaning up contaminate skin isn’t always simple, but it can be. For example, most cases of minor skin contamination can be cleaned up with soap and warm water. In fact, every time I’ve had skin contamination, soap and water has worked for me. It’s also possible to wipe down the contaminated skin with baby wipes or other cleaning-type wipes. Wiping down with a damp rag or sponge will often do the trick as well, and other specific circumstances (or specific compounds that you might be using) might call for more specialized products. No matter how you choose to decontaminate a person there are a few rules of thumb to keep in mind.
- Don’t do anything painful or uncomfortable. For example,
- Don’t use hot or cold water – keep it cool to warm.
- Don’t scrub with harsh substances (e.g. steel wool, scrub pads, wire brushes, etc. – and don’t laugh; I’ve seen all of these used).
- And above all, don’t do anything that will draw blood. Your skin acts as a pretty good barrier, keeping contamination out of your bloodstream – if you do something that breaks the skin then you’re simply scrubbing contamination into the blood, which is never a good idea.
- Count for contamination every several washes or wipes. As long as contamination levels are dropping then whatever you’re doing is working and you should keep doing it. If contamination levels stop dropping then what you’re doing is no longer working and it might be time to try something else.
You also have to understand when it’s time to follow-up or call for help. And “call for help” is not necessarily as dramatic as it might sound – that can simply mean calling a consultant. There are a number of possibilities in this category – here are a few of the more common.
- For example, you might consider performing a thyroid count for every case of skin contamination with radioactive iodine, or performing urine bioassay if skin contamination exceeds, say, 10,000 cpm (you’ll have to determine what these “trigger” levels are for the nuclides you’re using).
- You might also consider contacting a consultant to determine the possibility of uptake and/or to calculate skin dose if skin contamination exceeds a given count rate.
- You (or, more likely, your consultant) might have to calculate radiation dose to the skin if contamination levels are sufficiently high. Duke University has an online calculator to help you with this. For more complicated cases, you can also use a program called Varskin, which is quite possibly the best software available for this purpose.
- You’ll also have to contact your regulators if you (or a consultant) determine that a person has exceeded 50 rem to the skin.
Finally, you’re going to have to document what happened and how you responded to it. Start with a short description of the circumstances causing the skin contamination (e.g. liquid splashed on the skin) and write down the number of counts you measured as well as the instrument used for the measurement (e.g. 45,000 cpm measured with a GM pancake probe). You should also briefly describe the decontamination procedure (e.g. washed with soap and water for five minutes) and the results (e.g. contamination reduced to less than 100 cpm above background). And note any follow-up measures or samples that were taken (e.g. performed urinalysis to check for uptake) and the results.
Finally, let’s put all of this in perspective. There are times that skin contamination can be damaging – the skin can be harmed from a sufficiently high radiation dose. But most of the time skin contamination is more of a nuisance than a risk. You have to take it seriously; you need to decontaminate the affected area, you need to try to get an accurate count rate to see how bad it might be, you need to document everything, and you need to know when to call for someone to give you a hand. But you don’t have to panic! Take a deep breath, break out your procedures and your supplies, and work methodically and you (and the person who was contaminated) should be OK!