This article is part two of a two-part series on radiation therapy. Read about Brachytherapy: Targeted Internal Radiation Treatment in part one to see how these complementary techniques are used in cancer care.
Hey Doc – one of my buddies at work has cancer and his oncologist recommended radiation therapy. Can you tell me how that works? Thanks!
As I mentioned in the last post, radiation has been used in treating cancer for over a century with two primary approaches – inserting radioactive sources or medications into the body is the family of treatments I discussed the last time and, in this post, I’ll go over the other…producing a beam of radiation from a machine or an external radioactive source and aiming that at the cancer. This is called “external beam therapy.” A while back I wrote about how linear accelerators (LINACs) produce radiation that can be used to treat cancer, so I won’t go into that again here. But there are other ways to produce a beam of radiation and to use it therapeutically, as well as methods for aiming and shaping the beam to deliver maximum dose to the tumor and minimal dose to nearby healthy tissues. That’s what we’ll discuss here.
Producing the beam
In addition to producing beams of high-energy x-rays in a LINAC, we can produce beams of protons, beams of electrons, beams of gamma rays, and even beams of neutrons, neutrinos, muons, heavy ions, and all sorts of other types of radiation. Most of these aren’t used for cancer therapy; some of them – protons, electrons, and gamma rays – are, and doctors are finding uses for other types of radiation as well. For now, let’s talk about the ones that are used most frequently.
Gamma beams are the easiest to produce – just take a radioactive source and, instead of putting it inside a person’s body, put it inside a shield with a port the radiation can pass through. When the port is covered by lead (or depleted uranium or tungsten) the beam is contained; to produce the beam, simply aim the port at the location of the cancer and uncover it.
Producing electron beams is also fairly simple – Roentgen knew how to do that in 1895, which is how he was able to produce x-rays. A Crookes tube, invented in 1870 as a way to investigate the properties of gases, shoots electricity through a vacuum – the “electricity” is simply a beam of electrons that are given off by an electrode at one end of the tube and that are attracted to another electrode at the other end. Today, we can aim that beam of electrons at shallow cancers such as some skin cancers, or it can be aimed at a metal target (e.g. tungsten) to produce x-rays to attack cancers deeper in the body. Mere child’s play!
Proton beams are almost as easy to produce – a proton is simply a hydrogen atom that’s been stripped of its electron. Like electrons, these protons are then accelerated by magnetic fields and shot into a tumor. The biggest problem is that protons are about 2000 times as heavy as electrons so it takes more energy and larger equipment to get them up to a useful energy. But it can be done!
OK – we’ve got a beam! The question is what to do with it.
Unless it’s a skin cancer that’s being treated, the beam will first strike the skin and subcutaneous tissues and it will do what ionizing radiation does – knock electrons off of atoms. These secondary electrons have a relatively short range in tissue and they deposit their energy a little more deeply in the body. The key is to focus the incident beam at the right depth so as to maximize dose to the tumor from the secondary electrons and the primary beam.
Shaping the beam
I’ve mentioned repeatedly in these two posts that one of the things the doctors are trying to do is to minimize the radiation exposure to healthy tissues. One reason for this is to reduce the risk of producing a new cancer from the radiation used to treat the existing tumor, but on top of that, physicians are admonished to “do no harm,” and this includes not damaging tissues, even in the treatment of a disease, that are healthy unless there is absolutely no choice. Luckily, there usually is a choice – by shaping the beam of particles or rays before it reaches the body.
Multiple beams
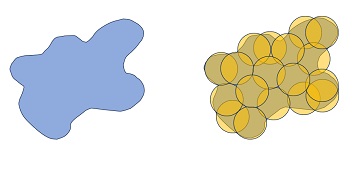
One way to do this is to use multiple beams – this is what the Gamma Knife does. A Gamma Knife holds as many as 200 individual radioactive sources arrayed around a hemisphere, each pointing inwards, each in its own shield and each with its own shutter. The radiation oncologist and medical physicist develop a treatment plan to use specific beams, placing the patient such that the uncovered beams intersect at the site of the tumor. What’s cool is that the beams need not intersect at a single point – by carefully positioning the patient, the beams can cover even irregularly shaped areas in three dimensions. And, by using multiple beams, the only tissue that receives a high dose of radiation is the area being treated – where the beams converge.
This technology has been in use for nearly 60 years, growing more popular with the addition of more-precise medical imaging and more-capable computers for treatment planning. One drawback to this system is that it requires maintaining a radioactive materials license for a large number of radioactive sources; another is that, unlike machine-generated radiation, radioactive sources can’t be turned off, they can only be shielded. Gamma knives are primarily used for cancers and other ailments in the head.
Simple Collimation
The simplest form of beam shaping is called collimation – putting a shield of an appropriate material (e.g. lead to shield photons) in the path of the radiation, into which an aperture has been milled with the same shape as the tumor to be treated. Thus, the part of the beam that will irradiate the tumor is allowed to pass through and the healthy tissues are spared exposure by the shielding.
Multileaf collimators
Another way to focus a beam of high-energy photons (e.g. x-rays, gamma rays) is to use lead shielding – specifically, lead shielding with a carefully shaped aperture that lets the radiation through in a shape that conforms precisely to the shape of the tumor. Since all tumors are shaped differently this requires shaping a custom aperture for each tumor to be treated – if the beam is to be applied from more than one angle, each angle requires a different outline. Rather than designing a number of different shields to cover all the possibilities, radiation oncologists use a device called a multileaf collimator – a device that uses a large number of individual sheets of lead, each of which can be precisely positioned to shape the beam so that it precisely irradiates the tumor. Not only that, but the beam can be moved around the body to irradiate the tumor from multiple angles so that the only part of the body receiving a high dose of radiation is the tumor itself. With a large number of sufficiently thin leaves virtually any shape can be covered, including the changing shape of a tumor being irradiated from a different angle.
Magnets
X-ray and gamma ray photons don’t have any electrical charge and the beam can only be shaped by putting shielding in the path of the beam. Electrons and protons, though – they’ve got an electrical charge, meaning that we can use magnetic fields to help focus, shape, and steer the beam they produce, just as the magnets in the old cathode ray-style computer monitors and television sets scanned the electron beam to paint the screen with the graphics, words, and images we used and watched..
Proton beams are an interesting case in point. Using powerful magnets, a stream of protons can be confined into a thin “pencil” beam that is scanned back and forth across the tumor, using an MRI of CT scan to guide the beam, painting the tumor in protons. Here, too, having precise control over a narrow beam makes it possible to irradiate only the tissues that are causing the problems.
That’s all I’ve got – at least, all that will fit into a few posts of modest length. There are plenty more details – following the links I’ve put in this piece and the last can take you to pages with additional information. Oh – and, if nothing else, you’ve likely noticed there’s a large number of treatments out there, each with its strengths and weaknesses; your friend is also likely to find out that there are differences from cancer to cancer that make some more amenable to one form of treatment or another, or that might respond best to a combination of treatments. This is where your friend really needs to talk with his doctors – learn what he can from them, find out why they recommend one approach over another, ask about the doctors’ experience with other cancers like his. Putting all of this information together, he can then decide which course of treatment he’d like to choose.
This article is part two of a two-part series on radiation therapy. Read about Brachytherapy: Targeted Internal Radiation Treatment in part one to see how these complementary techniques are used in cancer care.