Hi, Dr. Z – so I’ve been reading some of your posts about nuclear medicine and medical radiation safety and I realize I don’t really know how all of this works. Can you tell me why injecting radioactivity into a person can help figure out what’s wrong with them, and how you we go from injecting the radioactivity to finding a health problem (or a health non-problem)? Thanks!
You know, that’s a really good point. I’ve just been taking it for granted that everyone knows how nuclear medicine works, and that’s clearly not a correct assumption. So let’s see what we can do to help clear up some of this stuff.
Say a doctor has a patient who’s lacking energy and they’re trying to figure out why. At some point the doc might wonder if the patient might have an under-performing thyroid gland – the thyroid (among other things) can affect our metabolism and energy levels. And it turns out that the thyroid sucks up iodine (this is why iodine is added to salt). Knowing this, the doctor can inject some radioactive iodine into the patient’s bloodstream, knowing that the radioactivity will collect in the thyroid – after waiting an hour or so for the iodine to collect in the thyroid gland the doctor can measure the amount of iodine that’s been absorbed to get an idea of how effectively the thyroid is taking up iodine. And with a gamma camera the doctor can even look to see if there are nodules in the thyroid that are taking up more or less of the radio-iodine. Studying these gamma images can help the doctor to see if the patient has any of a number of thyroid diseases – including thyroid cancer.
Doctors can examine more than just the thyroid. I recently had some Tc-99m injected into my veins to let my cardiologist take a look inside my heart – using gamma cameras my doctor was able to tell whether or not blood was reaching the entire heart muscle (a blocked coronary artery will deprive parts of the heart of blood, causing that part to show up on a gamma camera scan) as well as to see how efficiently the heart was pumping blood. And several years earlier I inhaled an aerosol containing Tc-99m to see if I had any obstructions in my lungs.
There are other radiopharmaceuticals that will show hairline bone fractures, blood flow in the liver, cancer cells in the brain, and much more. The principle of all of these is the same – adding radioactive atoms to chemicals that are preferentially absorbed by a specific organ or by cancer cells makes it possible for doctors to see problems that are inside the body – the reason they can do this is because the radiopharmaceuticals emit gamma radiation, which can penetrate through the body’s tissues to be imaged by a gamma camera.
Of course, if radioactivity can concentrate in an organ (or a tumor) to help a doctor get an image of it then a larger dose of radioactivity might be able to concentrate in diseased tissues (such as tumors), delivering enough radiation dose to destroy the bad cells. This is another use for radiopharmaceuticals – a low dose of radio-iodine can reveal cancer’s presence and a higher dose can destroy the thyroid tissue, including any cancer cells it contains. Not only that, but if the thyroid cancer has metastasized, the radio-iodine will be absorbed by the metastases, destroying them as well; this is a therapeutic use of nuclear medicine.
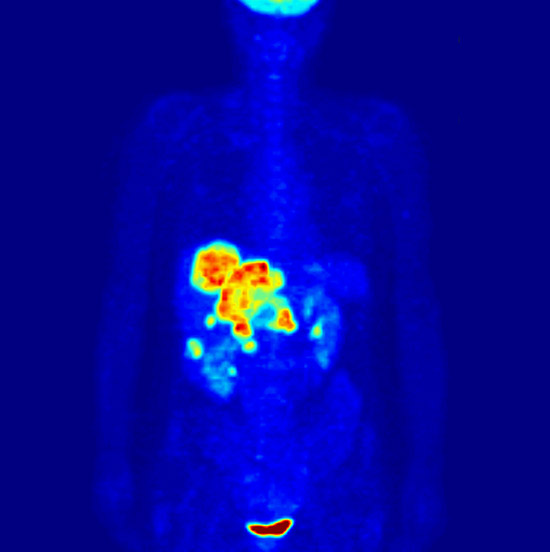
Another form of nuclear medicine involves the use of radionuclides that emit positrons – the antimatter equivalents of electrons. Antimatter is not just on Star Trek – it can happen within a patient’s body. And when the positrons meet up with a regular electron the two particles annihilate each other, turning into pure energy in the form of two gamma rays. Using our ever-popular gamma cameras, these gamma rays can be used to see where the positron-emitting radiopharmaceutical has collected. In many cases, the positron emitters are attached to sugar molecules; because cancer cells are dividing rapidly they use a lot of sugar for energy; labeling sugar molecules with radioactive isotopes gives the doctors a radioactive molecule that’s taken into quickly growing cells – since those include cancer cells, it gives doctors a way to see cancers and metastases inside the body. This is called positron-emission tomography – PET for short.
What makes nuclear medicine possible – at least in today’s high-resolution style – is gamma cameras. Without going into all the details (although, if you’re interested, you can find some of those details at https://en.wikipedia.org/wiki/Gamma_camera or https://radiopaedia.org/articles/gamma-camera) a gamma camera lets the physician see where in the body the gamma rays are coming from – knowing where they’re coming from, the doctor can identify nodules, tumors, and other features where the radioactivity collects – or that it avoids.
What can make this really cool is when we combine the nuclear medicine images (which show where the radioactivity is being absorbed and used by the body) and an x-ray or CT image (which shows where the bones, organs, and other parts of the body are). Combining a PET scan with a CT scan (called PET/CT) shows the physicians not only where a tumor might be, but also the organs, bones, and other structures that are nearby.
So this is a nutshell summary of how nuclear medicine works. And, as with so many of the questions I receive, there’s a lot of additional information that could be added, but I’ve got to stop short of book-length. But there is one other thing I should talk about a little – what a gamma camera is and how it works. Because without this key piece of technology we couldn’t do nuclear medicine very effectively.
It starts with a relatively thick piece of lead – thick enough to block most of the radiation that strikes it. There are a LOT of holes drilled through the lead – a gamma that can pass through a hole will pass through the lead but, because the lead is fairly thick, the gammas will only pass through if they’re lined up exactly right – if the hole is directly over the point from which the gammas are emitted. On the other side of the lead is a detector that counts the gammas coming through the lead and that’s able to tell which hole each gamma ray passes through. As with film or digital cameras, locations that have many gammas passing through look brighter than locations that detected fewer gammas – gradually the detector builds an image showing where the radionuclide is concentrated. The closer together the holes are, the better the camera’s resolution.
So that’s pretty much how it works – radiopharmaceuticals are given to the patient, accumulating in the organ of interest or at sites where that particular chemical is absorbed by the body. Those areas become more radioactive, giving off gamma rays; scanning the patient with a gamma camera lets physicians see where the radiopharmaceutical is accumulating. Easy peasy!