Yo, Doc Z! I was wondering if you can tell how they make x-rays and control the dose from them. Every time I have an x-ray I’m wondering about that stuff, but I don’t want to bother the tech…but I’m curious.
Ah – good question! And there’s a bit more depth to this than you might think! So let me start with how x-rays are produced, the different parameters that can be adjusted (and how the adjustments affect dose), and what we can do to try to keep dose to the patient as low as possible. And I should say that a LOT of people get x-rays every year via x-ray and CT procedures; more if we include fluoroscopy and CT scans. But I’m getting ahead of myself – let’s go back to how x-rays are produced and we’ll take it from there. There’s also a nice explanation of this (with pictures!) at https://www.radiologymasterclass.co.uk/tutorials/physics/x-ray_physics_production#top_1st_img.
It starts with a filament – a wire made of tungsten or some other suitable metal, through which an electrical current is passed. As the electrical current passes through the wire, some of the electrons “evaporate” off the filament; when this happens they’re drawn towards an electrode that’s got a fairly high positive electrical charge applied to it. The electrons are accelerated towards this anode by the high voltage, slamming into it at a high speed. When that happens, the electrons are deflected by the electrical field of the electrons surrounding the atoms, or by the electrical field of the protons in the atomic nucleus. This deflection causes the electrons to change direction or they collide with electrons surrounding the atoms in the target and, when that happens, they emit x-ray photons.
So…this gives us a chance to look at some of the parameters that help to determine the radiation dose to the person (or pet) being x-rayed and to others who might be in the vicinity.
- Voltage (kVp) is the voltage applied to the anode; a higher voltage on the anode produces electrons with a higher energy, producing higher-energy x-rays that are more likely to pass through the body and, if they don’t deposit their energy in the body then the total dose is reduced. So, seemingly paradoxically, increasing kVp results in lower radiation exposure.
- Current (mAs) is a measure of electrons flowing past an arbitrary point in space; a higher current (more mAs) means that more electrons are flowing, more are evaporating off, and more are producing x-rays when they strike the target and producing a higher radiation exposure
- Filtration (mm Al) is a little more involved. The x-rays that are produced have a wide range of energies from high to low. The low-energy x-rays don’t have enough oomph to pass through our bodies – they’re absorbed by the tissues of our body. This means that they produce radiation dose, but they don’t provide any diagnostic information. By passing the x-rays through a thin sheet of aluminum, the lowest-energy x-rays – the ones that are absorbed but provide no diagnostic information – are filtered out, reducing radiation dose and improving the quality of the x-ray. The equivalent of a few mm of aluminum of filtration will “harden” the beam
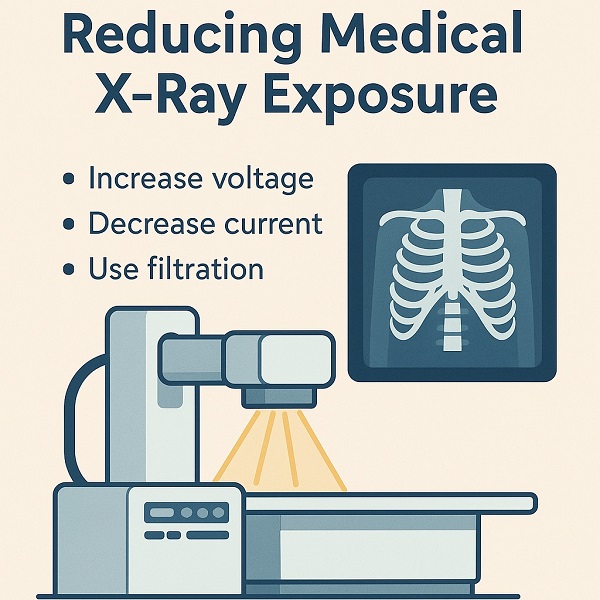
Putting all of this together, it seems that increasing kVp, reducing mAs, and increasing the mm of aluminum in the filter should reduce radiation exposure to the patient. Easy! Except that there’s a little more to it than that. Let’s start with the part of the body that we’re interested in imaging.
Imaging hard tissues (bone and teeth, primarily) is easy – because of their density they’ll stop most of the x-rays at even the highest energies. So if we’re looking for a broken bone we can ramp up the kVp and the filtration to get the hardest (highest-energy) beam possible, minimizing dose to the patient. But what if the goal is to look for, say, a tumor? Most of the body’s tissues have a similar density so, to a beam of hard x-rays, a tumor will look a lot like the tissue it’s surrounded by. The way to see soft tissues is to use lower-energy (“softer”) x-rays that are absorbed more by, say, a tumor than by the organ in which it’s growing. Imaging soft tissues can produce more radiation exposure to the part of the body being imaged, but that’s better than not having important diagnostic information such as the presence of a tumor.
The beam current – mAs – is a little easier; a high mAs means that there are a lot of electrons flowing through the filament and striking the target. More electrons in the beam means more electrons striking the target where they produce more x-rays. All else (i.e. kVp and filtration) being equal, a higher mAs means a higher radiation dose. With mAs…think of mA part as equivalent to the brightness of a flashlight – the higher the mA the “brighter” the beam; the longer the “light” is on (the “s”), the better the overall view. The goal is to have a “bright” enough beam (mA) for a long enough period of time (s) to get a good image, without excessive radiation exposure. I should also mention that some situations call for more or less mAs than others. A thin patient, for example, has less tissue and, therefore, less shielding and requires fewer mAs than does a heavy patient.
So getting back to your question, the way that x-ray techs control your exposure is by choosing the proper technique – the proper combination of x-ray energy (related to kVp and mm of aluminum of filtration) and the total number of x-rays produced (related to mAs).
Finally, you can find more information on the Image Gently website. Image Gently is an organization dedicated to minimizing radiation exposure from radiography procedures. Their website gives additional information about how to do so, aimed at radiology techs and physicians.